Visible blood in urine can be due to many reasons, such as infection or trauma, but it may also be a symptom of Urological cancer and it is important it is investigated thoroughly.
In 2019, the Royal College of Surgeons in Ireland in partnership with the National Clinical Programme in Radiology and the National Clinical Programme in Urology Surgery agreed to collaborate in a key quality improvement initiative to develop Rapid Access Haematuria Pathways. In Beaumont Hospital, a visible haematuria pathway was established in 2019 to ensure timely access to for patients with haematuria to be assessed and have diagnostic tests performed. Since then referrals to the service have risen annually from 161 to 483 new patients in 2023 being seen by the service.
How does the pathway work?
- Initial Assessment: This involves a taking a detailed medical history inquiring about symptoms like pain, frequency, or urgency of urination, and any risk factors for urological problems. Risk factors for urological problems (smoking history, occupational exposures, previous cancer treatments radiation to pelvis, certain chemotherapies, family history, chromic bladder irritation etc.)
- Urinalysis and Urine Culture: A urinalysis is a test that checks the physical, chemical, and microscopic properties of urine. It can help identify the presence of blood cells, infection, or other abnormalities. A urine culture is a test to identify any bacteria or other organisms present in the urine, which can cause infections.
- Blood tests: Blood tests don’t directly diagnose the cause of visible haematuria. They are used along with other investigations to build a more complete picture and guide further management. Blood tests can include kidney function tests, complete blood count (CBC), clotting tests, prostate-specific antigen (PSA) tests.
- Imaging Tests: Depending on the patient’s age, risk factors, and initial findings, imaging tests like kidney ultrasound, CT urogram (intravenous pyelogram), or cystoscopy might are recommended.
-
- Kidney ultrasound: This painless procedure uses sound waves to create images of the kidneys, ureters, and bladder. It can help identify any abnormalities in these organs, such as kidney stones or tumors. Click here for more information.
- CT Urogram: This is an X-ray imaging test that involves injecting a contrast dye into a vein. The dye helps to highlight the urinary system, allowing for a more detailed examination of the kidneys, ureters, and bladder. Click here for more information.
- Cystoscopy: This is a minimally invasive procedure that uses a thin, flexible tube with a light and camera on the end to examine the inside of the urethra and bladder. It can help to identify any abnormalities in these structures, such as bladder stones or tumours and is the gold standard investigation for bladder cancer
- Diagnosis and Treatment: Based on the results of the investigations, a diagnosis will be established. The treatment plan will depend on the underlying cause of the visible haematuria. In some cases, no treatment may be necessary. For others, treatment might involve antibiotics (for urinary tract infections), medications to manage kidney stones, or surgery (to remove tumours).
Following this pathway ensures a standardised approach to diagnosing visible haematuria, potentially leading to earlier detection and treatment of urological malignancies. This can significantly improve patient outcomes by:
- Increasing the likelihood of early-stage cancer detection: Early detection of urological malignancies allows for more effective treatment options and a better chance of cure.
- Reducing treatment morbidity: Cancers detected at earlier stages often require less invasive treatments, which can lead to fewer side effects and a quicker recovery time for patients.
- Improving patient survival rates: Early diagnosis and treatment are crucial for improving the overall survival rates of patients with urological malignancies.
Having a visible haematuria pathway ensures that patients with blood in their urine receive a prompt and thorough evaluation, ultimately leading to better patient outcomes.

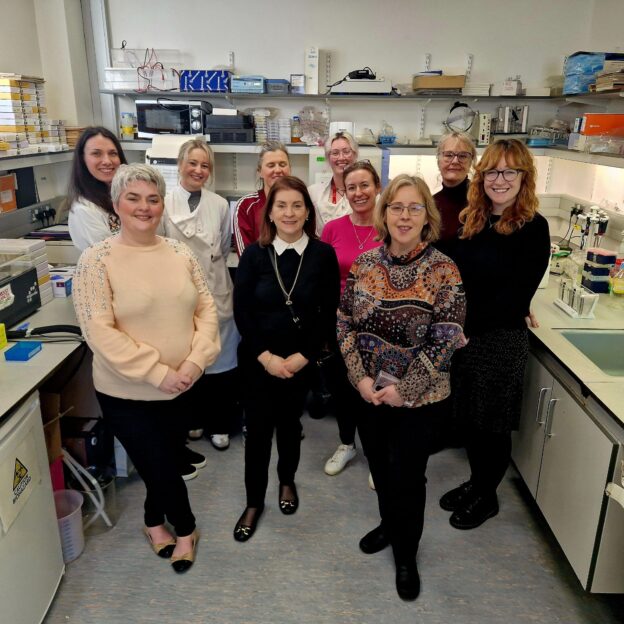
Urology Nursing Team: Angela Niland ANP Urology/Tx Retrieval
Karen Kelly ANP Urology/Tx Retrieval
Liana Keegan ANP Urology/Tx Retrieval
Clodagh Sharpe ANP Haematuria
Alison Doran CNS Penile, Bladder & Renal
Yemema Kurian CNS Urology









 Vicky Lunt – Principal Clinical Psychologist – “I left the lab feeling reassured that there are world class trials ongoing in Ireland. I am not sure how many people are aware of just how much passion and focus goes into the work of these researchers.”
Vicky Lunt – Principal Clinical Psychologist – “I left the lab feeling reassured that there are world class trials ongoing in Ireland. I am not sure how many people are aware of just how much passion and focus goes into the work of these researchers.” 








